
I’m getting a lot of phone calls from journalists about the California Department of Public Health’s COVID-19 vaccination plan, which you can find here in its entirety. The state vaccination plan consists of three phases (see the image below).
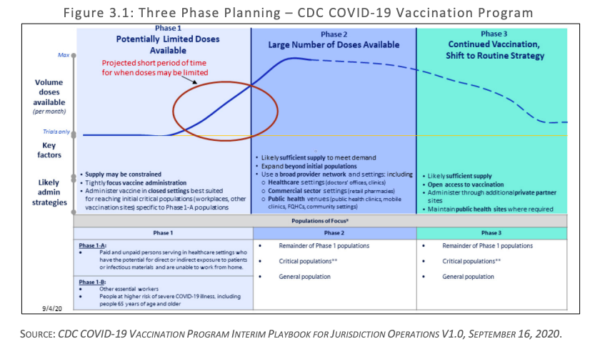
Phase 1, during which the state will have a limited supply of vaccines, focuses on critical populations in two subphases:
- Healthcare personnel likely treating patients with COVID-19 (Phase 1-A)
- Healthcare personnel likely to be exposed to COVID-19 (Phase 1-A_
- People at increased risk for severe illness or death from COVID-19 (Phase 1-B)
- Other essential workers (Phase 1-B)
California has an Allocation Data Team tasked with identifying these critical populations. CDCR is mentioned as one of the agencies whose datasets are going to be reviewed by the Allocation Data Team. Notably, one of the criteria for allocating vaccines is “identifying disadvantaged populations and communities that have been disproportionately impacted by COVID-19 in terms of higher rates of infection, hospitalization, and deaths.” To combat these well-documented disparities, California has developed a health equity metric and is working to improve the collection of race and ethnicity data associated with testing and cases.
Part and parcel of the vaccination plan is an effective communication strategy, which consists of outreach and education. The report explains how communication will be carried out:
With over 4,000 medical providers participating in California’s Vaccines for Children program and over 500 federally qualified health centers in our Vaccines for Adults program, a solid communication infrastructure exists for getting information and program updates to participating providers (program updates are sent electronically and also posted at https://eziz.org/ ). The CDPH Immunization Branch also employs field staff in five regions to serve as liaisons between provider offices and local health departments. These mechanisms, combined with the knowledge and relationships between local health care providers, pharmacies, and local health departments, have already established points of contacts and methods of communication. Additionally, local emergency preparedness programs have established close communication channels with first responder organizations, groups serving vulnerable populations and large employers throughout our state’s diverse counties. Local health departments have also been keeping close track on communities most adversely affected by COVID-19 and many have bolstered their responses to include specific outreach, education and mitigation efforts in those communities, establishing good relationships along that way that are paving the way for COVID-19 vaccine.We have also been working with the California Conference of Local Health Officers and the
County Health Executives Association of California to define and establish contacts for Multi
County Entities (MCEs). An MCE is a health system that has facilities in more than two California
counties to centrally support local implementation in all of its locations, set policy for all of its
facilities, order and store vaccine, has a centralized pharmacy, and has a demonstrated track
record in immunizing all of their staff. Northern and Southern California Kaiser Health Systems
are the two largest MCEs defined to date. Conversations are continuing to delineate more
MCEs and processes are being created and refined for how these entities will be registered in
our provider enrollment systems for vaccine ordering, allocation, tracking and reporting. MCEs
will become critical partners to immunizing in their communities and will be brought fully into all communication networks and monitoring infrastructures. We will augment these well-established networks with any additional input from our Community Vaccine Advisory Committee.Successful communication regarding critical population groups will start with clear guidance at the state level. The state will communicate to local health jurisdictions and MCEs about which and when specific critical populations should be receiving the vaccine. The state, in turn, will rely heavily on these local jurisdictions and multi-county entities to communicate directly with the providers for whom they will be approving allocations. The points of contact for these providers will be established through the provider registration process, which is discussed in further detail in Section 5.
Additionally, we will employ various communication methods to reach critical population groups. To communicate out to the groups that will be eligible for vaccination, we will send messages both from the local and state level about which categories of people should be vaccinated and, when. At the local level, emergency operations centers remain activated and will utilize well-established networks for reaching emergency responders and health care personnel. These well-established networks include Public Health and Medical emergency response partners, such as the Regional Disaster Medical Health Coordination and Medical and Health Operational Area Coordination programs. We will rely heavily on these networks as well as on statewide health care associations such as the California Hospital Association, the California Primary Care Association, the California Medical Association, local health care coalitions, and others. We will also rely on the California Immunization Coalition, our CCLHO and CHEAC organizations, EMS organizations (such as the Emergency Medical Services Administrators’ Association of California [EMSAAC] and the EMS Medical Directors Association of California [EMDA]), and many other professional associations. Emphasizing transparency and equity every step of the way, we will engage our Office of Health Equity, Governor’s COVID-19 Vaccine Task Force, Community Vaccine Advisory Committee members and other stakeholders to ensure that our communications are inclusive and that our strategies are in alignment with the best use of the vaccine at any given point in time.
This report, to me, raises a few points that are crucial to highlight at this particular time–and that require immediate action:
Prisons MUST be designated a vaccine priority site because of the nature of the interpersonal interactions.
Everything we know about the pandemic in prisons shows us that the rate of infections is much higher–approximately ten times higher–than the rate in California generally, and that mortality rates–even when adjusted for age–are much higher. Prison staff–correctional officers and prison workers–come in direct contact, and treat, incarcerated COVID patients just like healthcare personnel on the outside. Moreover, incarcerated people have not seen their families and loved ones since early March, when all visitation was halted because of the pandemic. Vaccinating them should be a priority.
Prisons MUST be prioritized because vaccinating behind bars protects everyone in CA.
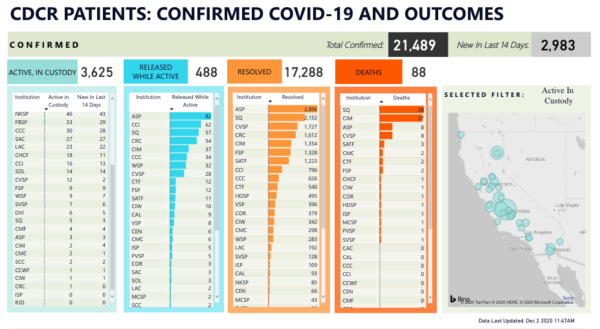
Moreover, it is imperative to understand the role that prison outbreaks play in the overall COVID picture of the state. As of today, only two CDCR facilities do not have any cases, and numerous prisons have serious outbreaks with hundreds of cases. The analysis we have provided throughout the last months shows a correlation between spikes in CDCR COVID rates and spikes in the surrounding and neighboring counties. Prioritizing prisons as vaccination sites protects everyone in California.
If equity is a consideration, incarcerated people should be first in line to get vaccinated.
The California Department of Health plan rightly emphasizes the need to factor equity in the distribution of vaccines, specifically through the prioritization of communities and race/class demographic groups who have born the brunt of infections and deaths so far. I can hardly think of a category of Californians who have, disproportionately, suffered more from COVID than incarcerated people. Vaccinating them first is not only prudent and worthwhile–it is fair.
At the same time, from a public health standpoint, outreach and education must begin now.
There are three main populations behind bars: incarcerated people, prison workers, and correctional officers. For reasons that I explained here, there is a serious, and understandable, trust and legitimacy deficit that could hinder effective cooperation in getting the prison population vaccinated, which stems from the fact that, for months now, whenever CDCR had an opportunity to earn trust and engender good will, they did exactly the opposite. CDCR have to start working on repairing this fundamental trust breakdown right now. The best way to do it is to drop all appeals, petitions, grandstanding, performative protestations about public safety, and resistance to the idea of releases, and let aging, infirm people go immediately home to their communities. Not only will this help get the pandemic under control much more quickly, it will go a long way toward reversing the understandable sense among the prison population that CDCR is deliberately indifferent to their plight, and thus will contribute to raising vaccination rates.
The other problem I foresee is with collaboration and buy-in from correctional officers. As I explained here, instead of raising the alarm about the health risks to their membership, CCPOA has been throwing millions of dollars at punitive voter initiatives. And as we learned from the Inspector General’s report and saw at the Assembly hearing, CDCR has not taken disciplinary steps against correctional officers who did not wear PPE when engaging with colleagues and with incarcerated folks. This could be the product of a members in thrall to a leadership that has been completely politically captured, Trumper-like COVID denialism among the rank and file, or both. But it needs to be firmly understood that COs who do not wear PPE and/or do not consent to getting vaccinated have no business working at CDCR facilities.
The problems with buy-in from these two populations need to be addressed immediately if there’s any hope of success with a vaccination program. Buy-in is an essential component of public health, and even if the entire prison population is prioritized–as well it should be–the vaccines are only as effective as their distribution in the population as a whole.
I will update this post with newspaper/media outlet articles about the challenges and urgency of vaccination programs in prison throughout the next few days.



No comment yet, add your voice below!